Dr. Nepuni Athikho
MBBS, DNB (Family Medicine), National Fellowship in Palliative Medicine,Family Medicine, Palliative & Home based Care Unit,CIHS, Dimapur, Nagaland
Pain is a common and distressing symptom in cancer. International Association for Study of Pain (IASP) defined pain as “An unpleasant subjective sensory emotional experience associated with actual or potential tissue damage or described in term of such damage”. Three fourths of cancer are painful and one third of cancer pain can be difficult to control, needing specialized care. This is the reason why National Comprehensive Cancer Network (NCCN) recommends active early involvement of palliative care in comprehensive cancer management right from the initial stage of cancer treatment.
Cancer pains can be acute pain or chronic pain. Chronic pains are more common in cancer. Chronic cancer pain shares the same pathway and similar characteristics of chronic non-cancer pain. We need to know that chronic and unrelieved pain takes the characteristics of a disease unlike acute pain which get better with time as healing of the wound or tissue damage repaired takes place. Chronic and unrelieved pain affects the psyche of a person and can change the whole personality of the sufferer. It also makes the patient seek the meaning of life and invoke God for healing and relief. Many cancer patients seek curative treatment, which remain elusive for many cancers and run into economic loss, causing considerable psycho-social pain to the patient and to the family as well. We need to know that curative cancer treatments are still not yet possible for many cancers. Moreover, most of the patients seek medical help in the advanced stage of cancer when curative treatment and surgery is impossible. Therefore, pain management leading to an overall improvement in the quality of life of the patient becomes a prime importance in comprehensive cancer treatment.
The common causes of pain in cancer are enumerate as follows: 1. Cancerous growth: The tumour cells produce chemicals like cytokines, interleukins, interferon, tissue growth factors, prostaglandins etc. These chemicals act as pain mediators or cause inflammation and produce pain. The cancerous growth may erode into the nerve ending, compress major nerve root or cause fracture of bone(s) due to metastasis or bleed in the tumour (HCC) or cause obstruction of the intestine and the ureter (Urine tube connecting kidney to the bladder).
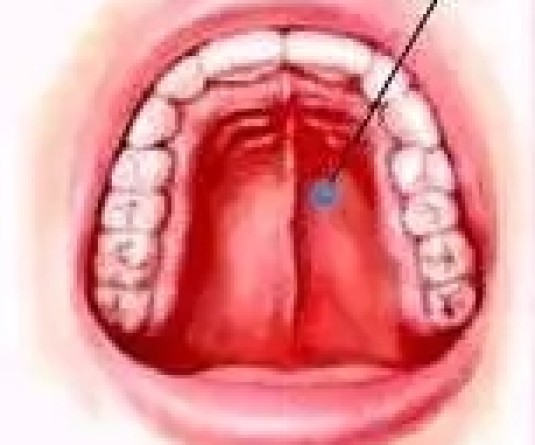
2. Treatment procedures: Investigative procedures, biopsy, surgery and mucositis, chronic pain related to chemotherapy drugs (Neuropathy), Radiation therapy(radiation plexopathy) etc.
3. Poor health (Debility): Poor nutrition, postherpetic neuralgia.
4. Co-existing disease: Diabetes neuropathy, Asthma.  The complexity of cancer pain demands proper evaluation, correct pain diagnosis, systematic analysis of the possible causes of pain, low cost affordable and accessible medicines, and a compassionate approach. Cancer pain management involves knowing the concept of “Total pain”, when psychosocial, physical, and spiritual distress combine to affect the patient's whole perception of pain. Also, chronic cancer pains affect the whole personality of the sufferer, not just the pain sensory nerve endings, family and relatives. Skilled communications and proper breaking of bad news facilitates patient and family acceptance of the reality of incurable disease, compliance to treatments and reduce uncertainty. Keeping these aspects of pain in mind, the palliative care team work together with the patient and the family members to ease physical pain, psychosocial and spiritual pain.
The complexity of cancer pain demands proper evaluation, correct pain diagnosis, systematic analysis of the possible causes of pain, low cost affordable and accessible medicines, and a compassionate approach. Cancer pain management involves knowing the concept of “Total pain”, when psychosocial, physical, and spiritual distress combine to affect the patient's whole perception of pain. Also, chronic cancer pains affect the whole personality of the sufferer, not just the pain sensory nerve endings, family and relatives. Skilled communications and proper breaking of bad news facilitates patient and family acceptance of the reality of incurable disease, compliance to treatments and reduce uncertainty. Keeping these aspects of pain in mind, the palliative care team work together with the patient and the family members to ease physical pain, psychosocial and spiritual pain.
The "Total cancer pain" means just a physician or a nurse giving pain medicines will not be enough, but, a palliative care team consisting of counsellor, chaplain, physiotherapists, and occupational therapists, working with the oncologists and other specialty teams have to work together with the patient and the family caregiver for optimal pain control. The difficult pain and non-responding pain to medicine need interventional pain management by an anaesthetist or pain interventional specialist.
Once proper assessment and evaluation is done, the palliative care physician decides the treatment based on the type of pain and patient preferences. The pain medicines are given according to the “WHO Pain Ladder”. Adequate pain control is achieved by following the golden rules of "WHO pain ladder" by clock, by mouth, by ladder, attention to details and individualized treatment. Standard pain assessment tools are used to assess the pain level before and after starting the pain control drug to gauge the efficacy of treatment. The pain assessment tools such as Wong-Baker FACES Pain Rating Scale, Numeric Rating Scale, FLACC(infants) enable the patient to quantify their pain as accurately as possible and enable them to control the level of pain and sedation. This process of pain management with careful and direct input from the patient is called Patient Control Analgesia (PCA).
Pain, the fifth vital sign which is also a somato-psychic phenomenon need a thorough assessment in all aspect by the treating physician or by the palliative care team. Psychologist or counsellors evaluate the patient to see any social, cultural belief, interpersonal conflicts, or conflict within the patient which might contribute to the distress and pain. The distress and adjustment disorders are treated with appropriate therapies like counselling, behavioral therapy, relaxation therapy, problem solving therapy and medicine in severe condition. Lastly, but not the least, spiritual pain plays a major role in cancer pain. In our Naga context, cancer treatment without prayer is incomplete and many patients search for meaning and answers for their suffering and this does not end in hospitals alone but goes beyond, from traditional healers to prayer centers. We are responsible to make the final journey comfortable, a painless dying process, wrap up smoothly and securedin their beliefs about the afterlife. Once we have done our best and as the patient enter into the final phase of their journey. We are in the End of Life Care(EOLC) phase. At this phase, palliative care provides emotional support, comfort and care to ensure physical comfort to the patient. The climax of palliative care is when patient utter words of satisfaction and gratefulness like " thank you, I love you, and Good bye". Once the patient dies, the palliative care team helps the family through the bereavementperiod by giving them emotional and psychological support.