MOHFW’s evidence based on Advisory on screening, diagnoses and management of ‘Mucormycosis.’ (Image Courtesy: MOHFW via PIB)
Centre’s drugs allocation suggests absence of infection in NE States
Morung Express News
Dimapur | May 19
Nagaland, so far, has not reported any case of ‘Mucormycosis’ or black fungus, a State official informed today, while the Centre’s list of allocation of COVID-19 essential drugs to be supplied from May 10-31 indicated absence of the infection in other North East States.
The list was annexed by the Union Ministry of Chemicals and Fertilisers (MoC&F) in a press release regarding monitoring and supply of COVID-19 essential drugs to States and Union Territories (UTs).
According to the list, a total of 44250 Amphotericine- B drugs were slated to be allocated to different states from May 10-31. It did not feature any states from North East or Union Territories.
Meanwhile as per the MoC&F data, maximum number of Amphotericine- B was scheduled for allocation in Maharashtra (16500), followed by Gujarat (15000) and Madhya Pradesh (3350).
According to United States’ Centers for Disease Control and Prevention, Mucormycosis “needs to be treated with prescription antifungal medicine, usually amphotericin B, posaconazole, or isavuconazole.” The BBC, on May 19, reported that Amphotericin-B was running was in “short supply” across states in India.
We have not received any reports so far, a Nagaland health official told The Morung Express on Wednesday, when queried on the issue.
The official, however, added that such infection is nothing new for Intensive Care Unit (ICU) patients and people on long term steroids.
“We should be very cautious as it is difficult to cure but hopefully shouldn’t be of a very big concern,” the official added.
Meanwhile, Assam-based news outlets on May 19 informed of a reported ‘Mucormycosis’ case in Assam. “The state of Assam witnessed its first case of black fungus infection Mucormycosis, in a Covid-19 patient in Guwahati,” the city-based The Sentinel reported on its website. According to reports, it was found in a youth on Wednesday morning at a private hospital and currently, he is said to be stable, it added.
What is Mucormycosis?
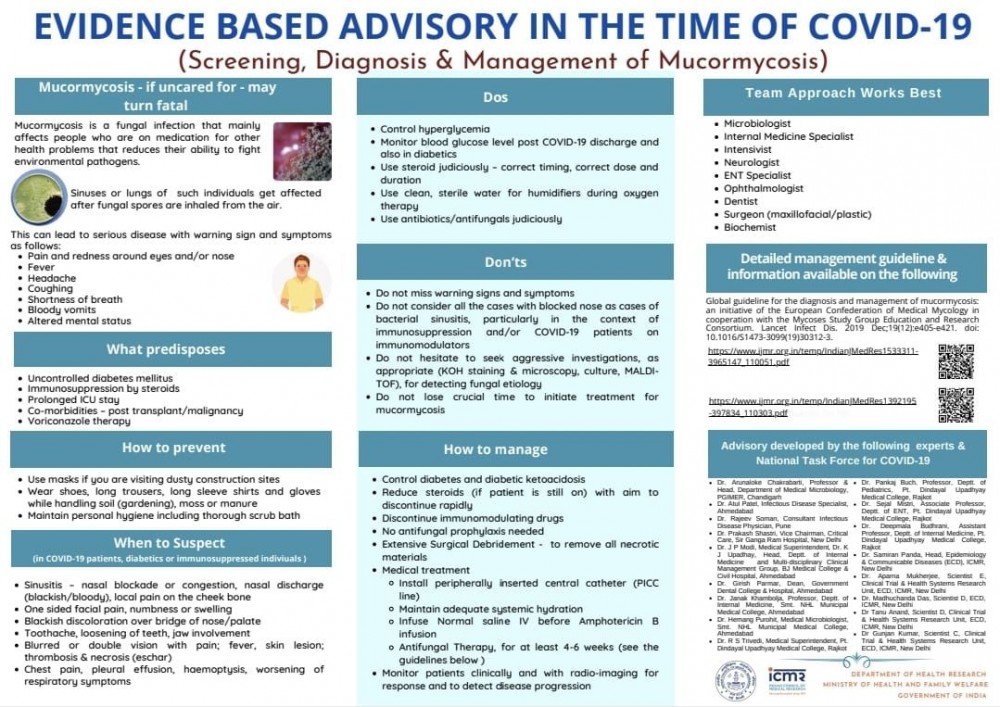
According to the Ministry of Health and Family Welfare (MOHFW), Mucormycosis or black fungus is a complication caused by fungal infection.
People catch mucormycosis by coming in contact with the fungal spores in the environment. It can also develop on the skin after the fungus enters the skin through a cut, scrape, burn, or other type of skin trauma, it stated in an advisory released on May 14.
The MOHFW then informed that the infection is being reported in a few COVID-19 patients during or post recovery and citing a statement given by the Health Minister of Maharashtra on May 12, added that more than 2000 people had already been affected by this fungal infection in the state while 10 people had even succumbed to it.
The disease is being detected among patients who are recovering or have recovered from COVID-19. Moreover, anyone who is diabetic and whose immune system is not functioning well needs to be on the guard against this, it cautioned.
Risk Group
According to an advisory issued by the Indian Council of Medical Research, the following conditions in COVID-19 patients increase the risk of mucormycosis infection:
Uncontrolled diabetes
Weakening of immune system due to use of steroids
Prolonged ICU/hospital stay
Co-morbidities / post organ transplant / cancer
Voriconazole therapy (used to treat serious fungal infections)
Relation with COVID-19
According to the MOHFW, the disease is caused by a set of micro-organisms known as mucormycetes, which are present naturally in the environment, seen mostly in soil and in decaying organic matter like leaves, compost and piles.
In normal course, the immune system successfully fights such fungal infections, however, COVID-19 affects the system and drugs used by infected patients like dexamethasone suppresses the immune system response, it said.
Due to these factors, COVID-19 patients face a renewed risk of failing the battle against attacks mounted by organisms such as mucormycetes, it maintained.
In addition, COVID patients undergoing oxygen therapy in ICU, where humidifier is used, are prone to fungal infection because of exposure to moisture, it added.
However, the MOHFW underscored that it does not mean that every COVID patient will get infected by Mucormycosis and the disease is uncommon in those not having diabetes but can be fatal if not treated promptly.
Chances of recovery depend upon early diagnosis and treatment, it added.
Common symptoms
Mucormycosis begins to manifest as skin infection in the air pockets located behind the forehead, nose, cheekbones, and in between the eyes and teeth, the MOHFW informed.
It then spreads to eyes, lungs and can even spread to the brain. It leads to blackening or discoloration over the nose, blurred or double vision, chest pain, breathing difficulties and coughing of blood, it said. The ICMR has advised that not all cases of blocked nose should be considered as cases of bacterial sinusitis, particularly during/after the treatment of Covid-19 patients. One must seek medical help for detecting fungal infection, it added.
Treatment
Treatment involves surgically removing all dead and infected tissue and in some patients, this may result in loss of upper jaw or sometimes even the eye.
Cure may also involve a 4-6 weeks course of intravenous anti-fungal therapy and it affects various parts of the body, treatment requires a team of microbiologists, internal medicine specialists, intensivist neurologists, ENT specialists, ophthalmologists, dentists, surgeons and others, the MOHFW said.
Prevention
Controlling diabetes is one of the foremost prevention methods suggested by ICMR and COVID-19 patients who are diabetic need to take utmost care, the MOHFW advisory noted.
Self-medication and over-dosage of steroids can result in fatal events and hence doctor’s prescription should be strictly followed, it said.
“Steroids should never be administered at an early stage of COVID-19. It should be taken only after sixth day of infection. Patients should stick to appropriate doses of the drugs and take the drug for specific number of days as advised by the doctors. Rational use of medicines should be ensured to avoid adverse side effects of the drug,” it added, quoting Member (Health), NITI Aayog, Dr VK Paul.
“Other than steroids, use of COVID-19 drugs such as Tocilizumob, Itolizumab also suppresses the immune system. And when these drugs are not used appropriately, it increases the risk, as our immune system fails to fight the fungal infection,” he added.
ICMR in its guidelines has also advised COVID-19 patients to discontinue immunomodulating drugs, a substance that stimulates or suppresses immune system, MOHFW said, adding that the National COVID-19 Task Force has revised the dosage of Tocilizumab to prevent any such adverse effects.
Maintaining proper hygiene can also help keep the fungal infection away and for patients on oxygen therapy, it should be ensured that the water in the humidifier is clean and is refilled regularly, it said.
After recovering from COVID-19, one should closely monitor and should not miss any warning signs and symptoms mentioned above, as the fungal infection is found to emerge even weeks or months after recovery, it added.






