IANS Photo
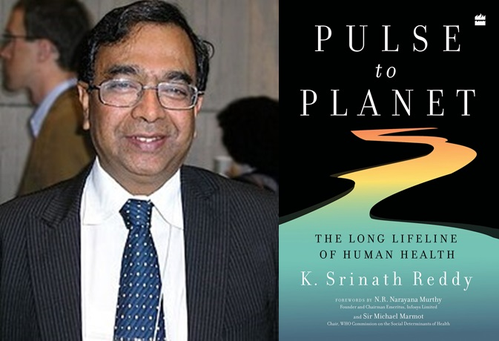
New Delhi, September 1 (IANS) Editor's Note: In a book that is both a gold mine of knowledge and a manifesto to make our planet a desirable bequest for the coming generation, eminent cardiologist and public health visionary Dr K. Srinath Reddy's ground-breaking book, 'Pulse to Planet: The Long Lifeline of Human Health' (HarperCollins Publishers), combines a breath-taking sweep with accessible wisdom to argue, in the words of Professor Lincoln Chen, formerly of the Harvard School of Public Health, that "human and planetary health depends upon both internal balance (homeostasis) and connectivity (people-to-people and people-to-environment)."
To continue with Dr Chen's summary of this must-have book: "Genes may be inherited but they are not fixed, influenced as they are by how they are expressed -- via epigenetics. Human genes are complemented by billions of bacteria that reside in our gut and skin. Nutrition is more than diets of individual nutrients, but also agricultural and food systems."
In this interconnected world, "health determinants are shaped by not only individual behaviour but also systemic economic, educational and social forces, especially powerful commercial interests. These forces are generating a fresh pattern of diseases; 'syndemics' like chronic diseases of obesity and new threats like COVID-19 and climate catastrophe."
Dr Reddy makes these myriads of connections in a language that is easy to grasp with a call to action against what he describes as the "rush to perdition". To quote Dr Reddy: "We need to veer away from this rush to perdition, not just to save those whose lives and well-being are at immediate risk but even more so to avoid the sin of shamefully scarring the lives of future generations." A call that our political class, policy makers, public intellectuals, teachers and students must take note of.
Excerpts from the book:
"The role of the infinitely small in nature is infinitely great." -- Louis Pasteur
Till recently, it was only a member of royalty who could refer to himself or herself in the plural 'we' instead of I. Not even persons with a multiple personality disorder would do that. Now it is clear that every human being can use the royal 'we'. It is not a universal assertion of the democratic spirit or a republican rejection of royal privilege.
It is just that human beings are now known to be minority shareholders in their own bodies, far outnumbered by other living organisms that cohabit and profoundly influence what happens to our bodies. ...
Science again, over the past two decades, has brought us a deluge of new information and provided astounding insights into the intimate relationship between human beings and a galaxy of microbes integral to the composition and functioning of the human body.
These are now graced with the collective name of the microbiome, conferred by Nobel Laureate Joshua Lederberg, who had earlier unravelled the intricacies of bacterial genetics but later became concerned over the indiscriminate demonisation of all microbes as a menace to be decimated.
Far from being regarded as dreaded enemies, many of the constituents of the microbiome are now seen as essential for human growth and survival. Disturbances in this crowded cosmos of microbes are being associated with a diversity of health disorders.
... each of us is only 43 per cent human, the rest of the cells in "our body" come from the microbiome that exists in teeming trillions on our skin, in our gut, mouth, airways, urogenital tract and secretions such as breast milk. Their genes far outnumber those of humans.
In contrast to the 22,000 human genes, the gut microbiota alone have about 3.3 million genes. Overall, of the panoply of genes we carry in our bodies, only 1 per cent are truly human genes.
'Helicobacter pylori' resides in our gut and is involved in signalling hunger or satiety to the brain. By regulating acid secretion in the stomach, this bacterium causes a decrease in ghrelin, a hormone that regulates appetite.
Absence of this microbe in the stomach elevates the level of ghrelin, which in turn increases the appetite, leading to excess consumption of food and obesity.
Consumption of high-fat diets reduces the microbiome volume, while favouring the growth of bacteria that stimulate fat deposition. Different results are observed when sterile mice, made germ-free by antibiotics, have faecal transplants from obese or slim mice. In the former case, the recipients develop obesity, compared to the latter who remain non-obese.
The integrity of the epithelial lining of the intestines seems to be dependent on the protection provided by the gut microbiome. The resident 'friendly' microbiome induces tolerance in the gut endothelium and participates in promoting gut immunity, endothelial stability and gut−brain interaction, while helping to keep out pathogenic bacteria.
Alterations in the microbiome (dysbiosis) are associated with gastrointestinal disorders such as inflammatory bowel disease, celiac disease, antibiotic-induced colitis and oesophagitis. Such disturbances may also be involved in carcinogenesis.
Much more unexpected is the growing evidence of the involvement of the microbiome in neuropsychiatric disorders such as depression, autism, Alzheimer's, dementia, Parkinson's and schizophrenia. It may seem far-fetched to think that the brain is affected by changes in the microbiome, but recent research is pointing in that direction.
Usually, the brain is protected from the direct invasion of microbes by the blood−brain barrier. However, the microbiome can still influence the brain through its effects on nutrients, hormones and various metabolites.
The microbes can also gain entry from the nose, climbing up the endings of the olfactory nerve, which is responsible for our sense of smell. Metabolites released by the gut microbiome act on the nerve endings of the vagus nerve that abound in the gut.
These signals can be transmitted to the brain.
The amyloid protein has long been linked to Alzheimer's disease as a key manifestation of brain pathology. The accumulation of amyloid and tau proteins became the hallmark of this disorder, which is the leading cause of dementia. Trials to target the amyloid with drugs have, however, proved to be disappointing failures. Coincidentally, the discovery that amyloid has potent anti-microbial properties led to the speculation that the amyloid deposition is a response of the brain to protect itself from microbes, which unfortunately results in self-harm in terms of severe cognitive decline.






