In this photo released by Xinhua News Agency, Yang Hongke checks on test samples at a testing lab of KingMed Diagnostics Group Co., Ltd. in Shijiazhuang in northern China's Hebei Province on January 9, 2021. (AP/PTI File Photo )

New Delhi, January 12 (PTI): In a first-of-its-kind study, researchers have analysed immune cells from the lungs of severe COVID-19 patients in a systematic manner and compared them to those from patients with pneumonia from other viruses or bacteria, findings which shed light on how the novel coronavirus infection spreads.
Instead of rapidly infecting large regions of the lung, the coronavirus sets up shop in multiple small areas and hijacks the host's immune cells to spread across the respiratory organ over a period of many days or even weeks, reveals the new study, published in the peer-reviewed journal Nature.
According to the research, the coronavirus infection leaves damage in its wake as it slowly moves across the lung and continuously fuels the fever, low blood pressure, and damage to the kidneys, brain, heart and other organs in patients with COVID-19.
The scientists, including those from Northwestern University in the US, noted that severe complications of COVID-19 compared with pneumonias caused due to other types of infections might be related to the long course of disease rather than more severe disease.
They performed a high-resolution analysis of the lung fluid of 86 COVID-19 patients on a ventilator and compared it with lung fluid from 256 patients on a ventilator who had other types of pneumonia.
The researchers took cells from patients' lung fluid and looked at the molecules present in these cells, enabling them to identify how these immune cells drive inflammation.
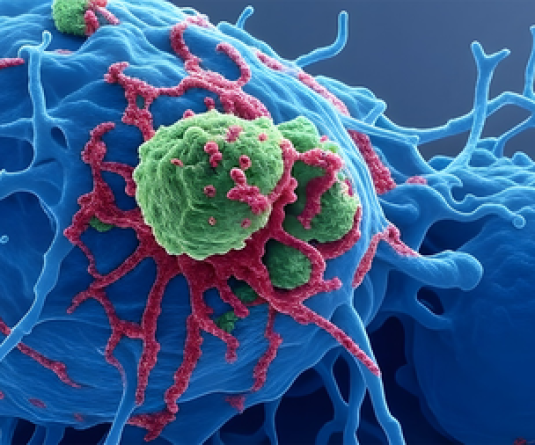
From the analysis, the scientists could identify critical drug targets in the immune cells -- macrophages and T cells -- to treat severe COVID-19 pneumonia and lessen its damage.
The results revealed that macrophages -- cells typically charged with protecting the lung -- can be infected by the coronavirus and can contribute to spreading the infection through the lung.
"Our goal is to make COVID-19 mild instead of severe, making it comparable to a bad cold," said study co-senior author Scott Budinger from Northwestern University Feinberg School of Medicine.
If COVID-19 patients are carefully managed and the health care system isn't overwhelmed, the scientists believe patients can recover better.
"These patients are very sick. It takes a really long time for them to get better. But If you have enough beds and health care providers, you can keep the mortality to 20 per cent. When health systems are overwhelmed mortality rates double up to 40 per cent," Budinger said.