Over 3.5 lakh Beneficiary Family Units estimated to be covered
Moa Jamir
Dimapur | September 8
With the objectives of protecting the citizens of Nagaland “against catastrophic health expenditure and reduce out-of-pocket expenditure” as well as part of fulfilling the Nagaland Sustainable Development Goal (SDG) Vision 2030, the Government of Nagaland (GoN) is planning for an ambitious universal health insurance scheme.
The scheme, first announced by Nagaland Chief Minister, Neiphiu Rio during the State Budget 2022-23 on March 22, appears to be near the horizon with the State Government issuing a short notice tender on August 31.
The tender invited competitive quotation from public and private insurance companies under the Insurance Regulatory Authority of India, to “carry on health insurance for implementation of Ayushman Bharat Pradhan Mantri Jan Arogya Yojna Chief Minister’s Health Insurance Scheme (AB PM-JAY CMHIS) for all eligible families in the State of Nagaland.”
As per the notice, the last date of receiving queries for the tender is September 14 and submission of bid ends on September 21. Opening of technical and financial bids is September 21 and the issue of notice of award (NOA) and acceptance of NOA are given as September 22 and 23 respectively.
The signing of insurance contract is September 23, added the notice issued by the Directorate of Heath and Family Welfare, State Health Agency (SHA) for AB PM-JAY CMHIS.
Meanwhile, on May 31, Chief Minister, Neiphiu Rio said that the State is contemplating to roll the CMHIS from October 1, 2022.
Scope of AB PM-JAY CMHIS
As per the ‘Request for Proposal’ (RFP) documents issued with the tender, the scheme is a convergence of existing Ayushman Bharat – Pradhan Mantri Jan Arogya Yojana, a scheme managed and administered by the Union Ministry of Health and Family Welfare and CMHIS.
The GoN wishes to embark upon Universal Health Coverage journey and desires to launch the Chief Minister’s Health Insurance Scheme (CMHIS) in convergence with the existing Health Insurance Cover for Deprived families under SECC 2011 through the AB PM-JAY, it said.
Accordingly, the AB PM-JAY CMHIS is aimed as a protection “against catastrophic health expenditure and reduce out-of-pocket expenditure by providing Insurance Coverage for hospital care to all residents of the State.”
It is a step towards fulfilling the Nagaland SDG Vision 2030 launched by the Chief Minister in August 2021 which envisaged that by 2030 the State “will ensure healthy lives and promote well-being for all ages by providing equitable, affordable, and quality healthcare services to the people of the state.”
The scheme will strengthen health systems and service delivery by increasing efficiencies, reducing fragmentation in existing health protection schemes, and improving service delivery and user experience, it added.
Eligibility and estimated beneficiates
Elaborating on the coverage, RFP documents informed all families under AB PM-JAY, including additional categories that have been extended benefits such as Building and other Construction Workers (BoCW) etc are included.
Meanwhile, under CMHIS, employees of GoN and other officials, and their dependents as well as serving Parliamentarians/Legislators are entitled for benefits under the existing Medical Reimbursement Scheme. It also includes pensioners and ex- Parliamentarians/Legislators.
Most importantly, the CMHIS is envisaged to benefit “any uncovered households with a valid Ration Card/ Permanent Resident Certificate (PRC) or Indigenous Inhabitant Certificate (IIC).”
Accordingly, by combining both, the AB PM-JAY CMHIS will offer universal health coverage.
A Beneficiary Family Unit comprises of “father, mother, husband, wife, brother, sister, son, daughter and includes grand-father, grand-mother, grand-child, adoptive father or mother, adopted son or daughter living together as a single household.”
For government servants and government retirees, the definition of family follows the Central Services (Medical Attendance) Rules 1944 – a government servant’s wife or husband as the case may be, and parents, sisters widowed sisters, widowed daughters, minor brothers, children, step children, divorced/separated daughters and stepmother wholly dependent upon the government servant and are normally residing with the government servant.
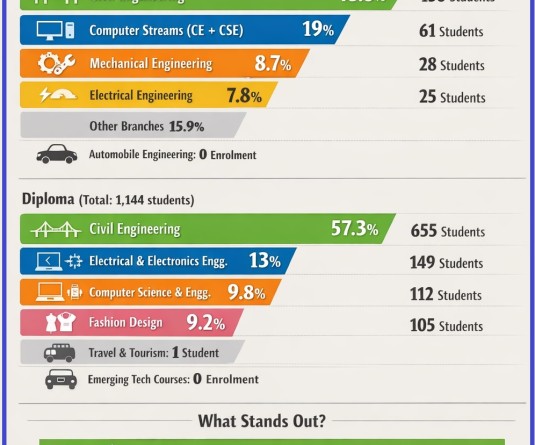
Meanwhile, as per the SHA estimate, there are 3, 50,453 Beneficiary Family Units, divided into five categories.
The first and second categories included minimum of 2,33,328 eligible families under AB-PMJAY and additional categories such as BoCW.
The third category are the employees of GoN currently employed at Pay Level 15 & above and serving Parliamentarians/Legislators (1,029); Pay Level 10 to 14 (6912) and Levels less than 10 (64,184).
The fourth is around 25,000 Pensioners while the fifth includes individuals not falling under any of the Categories 1 to 4, with around 20000 families.
Risk cover
Under the scheme, “Benefit Risk Cover or Benefit Cover” refers to the annual basic cashless hospitalisation coverage of Rs 5 lakh on a “family floater basis that all the insured families would receive...” In other words, under family floater basis, health insurance plan will extend the coverage to the entire family rather than just an individual, under whose name it is registered.
In addition, for beneficiaries belonging to the category CMHIS (EP) i.e., Employees and Pensioners of the GoN, are eligible for top up cover of Rs 5 lakh or Rs 15 lakh over and above basic cover, based on the financial viability of premium discovered.
Meanwhile, under Nagaland Health Benefit Package 2022, beneficiaries are divided in two categories: N-HBP 2022 for CMHIS (GEN) and N- CMHIS (EP).
Under the general category, approximately 1950 in-patient procedures across 27 major clinical specialties would be covered. The procedures will include both surgical and medical procedures and limited day-care packages, among others.
For CMHIS (EP), there were 1853 procedures listed, though they have additional benefit including in-patient care with differential room entitlement.
Based on the feedback and suggestions received from stakeholders, the procedure list may undergo revisions, additions, and deletions as the AB PM-JAY CMHIS progresses, the RFP documents stated.
More details will be available when the GoN formally rolls out the scheme.