Over 91% shortage of specialist doctors at CHCs in Nagaland
Moa Jamir
Dimapur | May 18
The number of health centres in Nagaland has considerably increased in the last 15 years, but the acute shortage of specialists and other skilled workers persists in CHCs, reflected the latest the Rural Health Statistics (RHS) 2020-21 released this month.
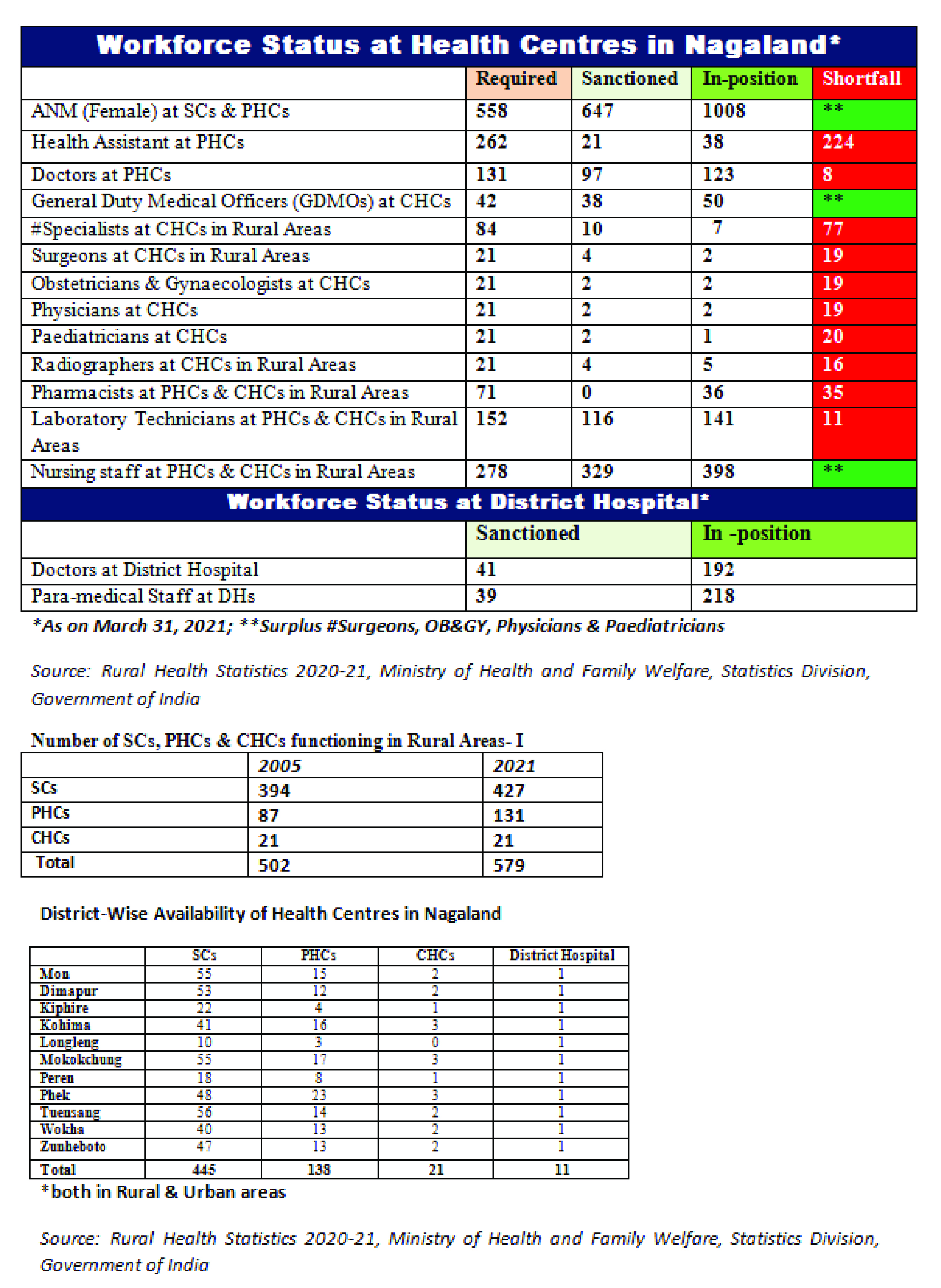
Overall, as of March 21, 2021, the number of Sub-Centres (SCs), Public Health Centres (PHCs) and Community Health Centres (CHCs) in rural areas of Nagaland increased from 502 in 2005 to 579 in 2021, the survey highlighted.
During the same period, 1,56,101 and 1,718 SCs were respectively functioning in rural and urban areas of the country, along with 2,51,40 (Rural) and 5,439 (Urban) PHCs, and 5,481 (Rural) and 470 (Urban) CHCs.
The public healthcare infrastructure in rural areas has been developed as a three tier- system with SCs at Tier III, the most peripheral and first contact point between the primary health care system and the community while PHCs at Tier II act as a first “contact point” between a citizen and a medical officer. The CHCs at Tier-I provide referral as well as specialist healthcare to the rural populace.
A PHC acts as referral unit for 6 SCs while the CHC serves as a referral centre for 4 PHCs as per the survey.
Persistent crisis at CHCs
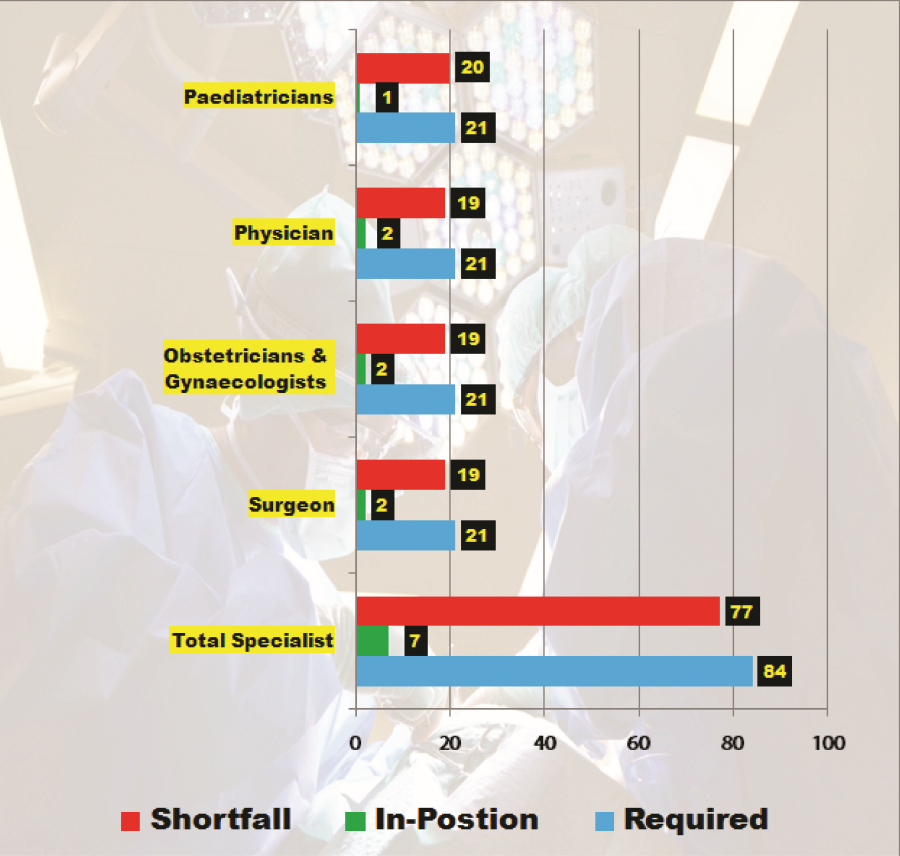
Overall, as of March 21, 2021, out of 84 specialist doctors required at 21 CHCs in Nagaland, only 7 were in position, indicating 91.66% shortfall of requirement prescribed by the Indian Public Health Standards (IPHS) norms.
A CHC is required to be manned by four medical specialists i.e. Surgeon, Physician, Obstetrician/Gynaecologists and Paediatrician supported by paramedical and other staff as per the IPHS norms.
Comparative data provided by the RHS indicated that the State Government has not done much to correct the shortfall in the last 15 years or so.
For instance, in 2005, the requirement and shortfall stood at 84, and since then, the State government has sanctioned only 10 specialist posts, out of which 7 were shown as filled on March 31, 2021, resulting in vacancy of 3, but an overall shortfall of 77.
Specifically, out of 21 Surgeons required at CHCs, only 2 were in position. The same goes for Obstetricians & Gynaecologists as well as Physicians.
There was only 1 Paediatrician in 21 CHCs across Nagaland as of March 31, 2021.
Nagaland was not alone in the shortfall of providing specialist doctors, but the shortage was much higher than the national average.
As per the survey, while specialist doctors at CHCs have increased from 3,550 in 2005 to 4,405 in 2021 across, there was a shortfall of 79.9% specialists at the CHCs as compared to the requirement.
Moreover, as compared to requirement for existing infrastructure, there is a shortfall of 83.2% of Surgeons, 74.2% of Obstetricians & Gynaecologists, 82.2% of Physicians and 80.6% of Paediatricians.
The shortage was not limited to specialists alone.
Overall, there were shortfall of 16 Radiographers, 35 Pharmacists, and 11 Laboratory Technicians at PHCs and CHCs in the Nagaland.
However, there was no shortfall of General Duty Medical Officers (GDMOs) at CHCs in Rural Areas in Nagaland.
Better status for PHCs
Meanwhile, the status of doctors at PHCs in rural areas showed a better picture, with shortfall reducing from 34 in 2005, to 8 in 2021.
As of March 31, 2021, out of 131 doctors required at PHCs, 123 were in position, resulting in shortage of 8.
As per the IPHS norms, a PHC has to be run by a medical officer supported by paramedical and other staff. Under NHM, there is a provision for two additional staff nurses at PHCs on contract basis.
In Hilly/Tribal/Difficult Area, a SC covers population of up to 3,000, while PHC and CHC cover 20,000 and 80,000 respectively.
Across India, allopathic doctors at PHCs have increased from 20,308 in 2005 to 31,716 in 2021, or around 56.2% increase. However, there was still a shortfall of 4.3% of allopathic doctors at PHCs, out of the total requirement at all India level.
Additionally, there were shortages of 224 Health Assistants at PHCs, with the just 38 in-position out of 262 as per the existing norms.
‘Mismatch’ figure
Incidentally, while there were shortages of others health professionals, there was no dearth of Auxiliary Nursing Midwives (ANMs) well as nursing staff at SCs, PHCs & CHCs in rural areas.
Accordingly, out of 558 ANMs required at SCs and PHCs in Nagaland, 1,008 were in position, which is nearly double the norm.
Again, while the required Nursing staff at PHCs & CHCs in rural areas is shown as 278, a total of 398 were in position in Nagaland as of March 31, 2021.
A look at the workforce status at District Hospitals also give a hint on why there could be shortage of doctors and other health professional at PHCs and CHCs.
As per the survey, out of 41 doctors sanctioned in the then 11 district hospitals in Nagaland, a total of 192 were in position.
In addition, out of 39 Para-medical Staff required at district hospitals across Nagaland, 218 were in-position.
Incidentally, hearing a Public Interest Litigation (suo motu), the Guwahati High Court Kohima Bench, on April 20, 2020 had directed the Principal Secretary, Department Health & Family Welfare, Nagaland to submit an “affidavit explaining as to why no medical personnel are posted at some of the medical centres.”