Dr Denchu Phom
CIHSR
What Are Haemorrhoids?
Haemorrhoids are swollen veins in the lowest part of your rectum and anus. Sometimes the walls of these blood vessels stretch so thin that the veins bulge and get irritated, especially when you poop.
Swollen haemorrhoids are also called piles.
Haemorrhoid is one of the most common causes of rectal bleeding. They are rarely dangerous, but you should see your doctor to make sure you don't have a more serious condition, such as intestinal disease, cancer, etc. Haemorrhoids often go away on their own, but treatment can also help.
Symptoms of Haemorrhoids:
Internal haemorrhoids
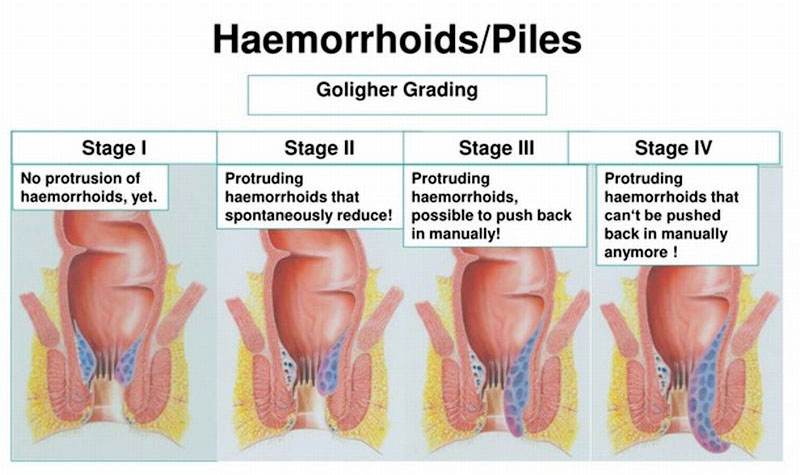
Internal haemorrhoids are far enough inside your rectum that you can't usually see or feel. They don't usually hurt because there are a few pain-sensing nerves in there. Symptoms of internal haemorrhoids include: blood on your poop, toilet paper after you wipe, or in a toilet bowl.
A tissue that bulges beyond the opening of the anal (prolapse). This can hurt, often when you're pooping. You may be able to see prolapsed haemorrhoids as moist bumps that are pinker than the surrounding area. They usually go back inside on their own. Even if they don't, they can often be gently pushed back to their place.
External haemorrhoids
External haemorrhoids are under the skin around your anus, where there are a lot more pain-sensing nerves.
Symptoms of external haemorrhoids include: pain bleeding,itching, Swelling.
A blood clot can transform purple or blue haemorrhoids. It's considered a thrombosis. It could pain, scratch, and leak. When the clot dissolves, you may have a little bit of skin remaining, which might get irritated.
What Causes Haemorrhoids
You may be more likely to have haemorrhoids if other family members, like your parents, have them.
Pressure building up in your lower rectum can affect the flow of blood and cause the veins to swell. This can happen from:
* Pushing during bowel Movements
* Straining when you do something that is physically hard, like lifting something heavy
* Extra weight, like obesity.
* Pregnancy, when your growing uterus presses on your veins
* A diet low in fibre
* Anal sex
* People who stand or sit for long stretches of time are at greater risk, too.
You may get them when you have constipation or diarrhoea that doesn't clear up. Coughing, sneezing, and vomiting could make them worse.
Haemorrhoids Diagnosis
Your doctor will ask about your medical history and symptoms. They will probably need to do one or both of these examinations:
Physical examination:
Your doctor will check your anus and rectum for lumps, swelling, irritation, or other problems.
Digital rectal examination:
Your doctor will wear gloves, apply lubrication, and insert a finger into your rectum to check your muscle tone and feel tender, lumpy, or other problems.
To diagnose internal haemorrhoids or rule out other conditions, you might need a more thorough test, including:
Anoscopy: Your doctor uses a short plastic tube called an anoscope to look into your anal canal.
Sigmoidoscopy: Your doctor looks into your lower colon with a flexible lighted tube called a sigmoidoscope. They can also use the tube to take a bit of tissue for tests.
Colonoscopy: Your doctor looks at all of your large intestine with a long, flexible tube called a colonoscope. They can also take tissue samples or treat other problems they find.
Haemorrhoids Treatment
Haemorrhoid symptoms usually go away on their own. Your doctor’s treatment plan will depend on how bad your symptoms are.
Home remedies: Simple lifestyle changes can often relieve mild haemorrhoid symptoms within 2 to 7 days. Add fibre to your diet with over-the counter supplements and foods like fruit, vegetables, and grains. Try not to strain during bowel movements; drinking more water can make it easier to go. Warm sitz baths for 10-15 minutes several times a day can also make you feel better. Ice packs can ease pain and swelling.
Nonsurgical treatments: Over-the-counter creams and other medications relieve pain, swelling, and itching. Check with your doctor if you still have symptoms after a week of using these.
Surgical treatments: If you have large haemorrhoids, or if other treatments haven’t helped, you might need surgery. Your doctor can use chemicals, lasers, infrared light, or tiny rubber bands to get rid of them. If they’re especially large or keep coming back, your doctor might need to permanently remove surgically.
Haemorrhoids Prevention
To prevent haemorrhoid flare-ups, take steps including:
* Eat fibrous foods: It helps food pass through your system easier. A good way to get it is from plant foods: vegetables, fruits, whole grains, nuts, seeds, beans, and legumes.
* Drink water: It will help you avoid hard stools and constipation, so you strain less during bowel movements. Fruits and vegetables, which have fibre, also have water in them.
* Exercise:Physical activity, like walking a half-hour every day, keeps your blood and your bowels moving.
* Don't wait to go. Use the toilet as soon as you feel the urge.
* Don’t strain during a bowel movement or sit on the toilet for long periods. This puts more pressure on your veins.
* Maintain a healthy weight.
* Don’t waste time in the toilet by playing games, reading.
What Not to Eat
Foods with little fibre can cause or make constipation (and therefore haemorrhoids) worse, so it's best to limit how much you eat of them.
• White bread and bagels
• Milk, cheese, and other dairy
• Meat
• Processed foods such as frozen meals and fast food
Watch the amount of salt you eat. It can lead to your body hanging on to water, which puts more pressure on your blood vessels. That includes the veins in your bottom that cause haemorrhoids.
Iron supplements can cause constipation and other digestive problems, so talk to your doctor before you take them.
How is a sitzbath done?

To take a sitz bath in a tub:
• Make sure your bathtub is clean. Fill a clean bathtub with 3 to 4 inches of warm water.
• Add salt or medicine to the water if advised by your healthcare provider.
• Gently lower yourself down into the bathtub and sit on the bottom of the tub. Don’t get into the bath unless the water temperature is comfortable.
• Hold on to a railing. Or ask for help from a family member, friend, or caregiver if needed.
• Sit in the water for 10 to 20 minutes.
• Add more warm water as needed to keep the water comfortable.
• Gently pat your anal area, perineum, and genitals dry with a clean towel. Don’t rub the area.
• Wash your hands. Put any ointment or cream on the area, if advised.
• Wash the bathtub or sitz bath bowl with soap and water after each use.
• Use a sitz bath 2 to 3 times a day, or as often as your healthcare provider advises.
The writer is Junior Consultant, Department of Surgery, CIHSR 4th Mile, Dimapur